E-cigarette or vaping was created with the intention of making a profit, changing market dynamics, and advancing various health ideologies.
There is yet insufficient data to determine if electronic cigarettes are safer than traditional tobacco cigarettes, despite the claims that they produce less smoke and less toxins.
Vaping from Medical Professionals’ Point Of View
The majority of medical specialists are generally against vaping. In particular, they advise against young individuals using nicotine products. Healthcare experts have made a deliberate effort for a long time to thoroughly inform all individuals about nicotine and tobacco use.
Although it’s possible that non-combustible goods provide fewer hazards, utilising all associated products is the only method to convince individuals to stop smoking nicotine, an addictive drug that also contains other potentially hazardous compounds. E-cigarettes might expose users to substances that aren’t present in tobacco cigarettes, among other dangers.

Image by Harvard Health
When treating tobacco smoking or vaping, the primary goal should be to stop the cycle of addiction. We are aware that stopping smoking improves respiration, heart health, and blood pressure regulation. Despite some worldwide signs that the use of e-cigarettes may lower the use of tobacco and operate as an alternative, this is the conclusion reached by the majority of healthcare professionals.
Vaping seems to be a rapidly growing fad. Some electronic cigarettes have been linked to the illegal trade in tetrahydrocannabinol (THC) goods that are tainted. Healthcare practitioners need to be diligent in keeping up with not just the hazards of vaping but also its proper and improper use as well as the most recent laws.
What are the risk factors?
Vaping is becoming more and more well-liked. Since some e-cigarettes provide nicotine while others do not, the hazards may vary. Instead, some vaping products contain flavouring, while others offer psychoactive ingredients like cannabidiol (CBD) or THC (the main psychoactive ingredient in marijuana).
Risk in using E-cigarettes was defined by the US National Academy of Sciences as: “Overall, E-cigarette aerosol contains fewer numbers and lower levels of toxicants than smoke from combustible tobacco cigarettes.”
The definition also said, “Overall, the evidence reviewed by the committee suggests that E-cigarettes are not without biological effects in humans.”
What are the biological effects?
The biological implications of vaping on people are still up for discussion. Knowing what potential harms these items can cause is crucial since it’s feasible that they’ll help individuals give up using combustible tobacco products.
Trading combustible tobacco products for electronic cigarettes doesn’t make much sense if vaping is just as risky or perhaps more so. Both have an equal risk of causing heart and lung problems.
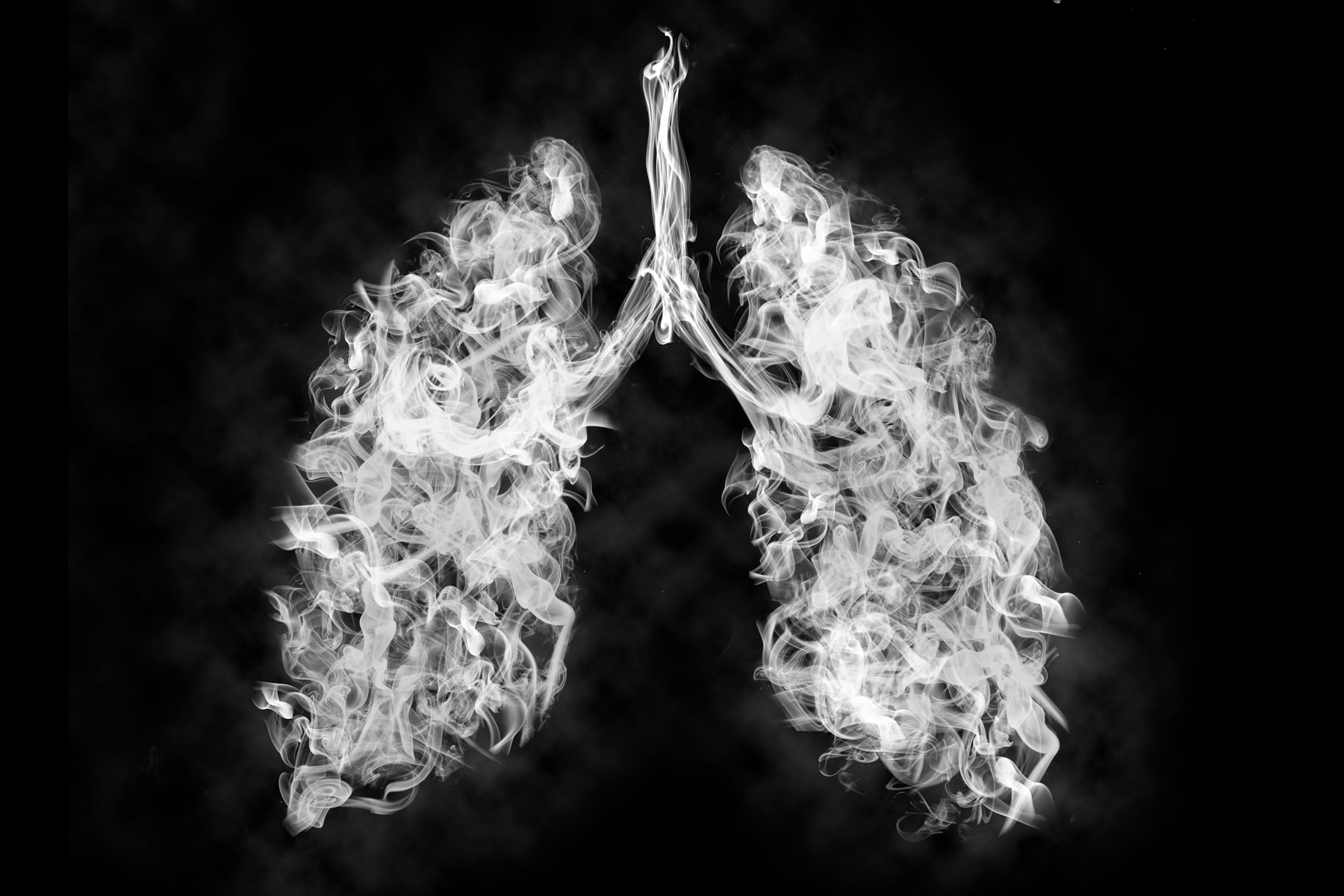
Image by USC News
The fact that you might not be familiar with the product’s ingredients adds another barrier to using e-cigarettes. Some producers assert that electronic cigarettes don’t produce the same toxins as conventional tobacco products, but research indicates that vaping exposes users to highly heated chemicals, particularly propylene glycol, which irritates both the throat and the lungs.
What are the effects on the heart and cardiovascular system?
Overall, e-cigarettes have a sharply unfavourable impact on heart rate (raised) and are linked to higher systolic and diastolic blood pressure measurements. Even if the effects aren’t as harsh as those of combustible tobacco products, they might still have negative impacts.
According to some investigations, e-cigarette use may increase oxidative stress and endothelial cell dysfunction, which may result in atherosclerosis. E-cigarettes may also interfere with platelet function, which raises the risk of blood clots or thrombosis.
According to the most current pre-clinical research, E-cigarettes cause conduction abnormalities and cardiac arrhythmias in mice. Vegetable glycerin and propylene glycol aerosols used in e-cigarette solvents seem to be the problem. As a result, there were increases in heart rate variability, bradycardia (slow heart rate), and bradyarrhythmia (slow irregular heart rate). The researchers came to the conclusion that the chemical components of e-cigarettes enhanced the chance of developing heart disease by producing cardiac arrhythmias and triggering autonomic reflexes.
Some contradictory findings could suggest that there is no underlying cardiac or cardiovascular risk associated with using e-cigarettes. Since these research focused more on E-cigarette consumption patterns and user experiences, they could be deceptive. Due to the numerous variations in sample size and E-cigarette usage in the research, it can be challenging to draw any conclusive inferences from the results.
E-cigarette use is still being evaluated by the US Federal Drug Administration, although there is currently no substantial regulation in place.



